Background: Oscillation and pulmonary expansion (OPE) therapy can decrease postoperative pulmonary complications in a general surgical population, but its effect after cardiac surgery has not been reported, to our knowledge. We hypothesized that using an OPE device after cardiac surgery before extubation would
[...] Read more.
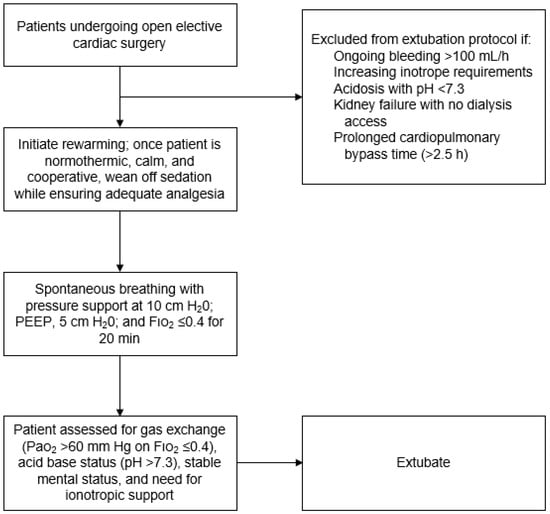
Background: Oscillation and pulmonary expansion (OPE) therapy can decrease postoperative pulmonary complications in a general surgical population, but its effect after cardiac surgery has not been reported, to our knowledge. We hypothesized that using an OPE device after cardiac surgery before extubation would decrease pulmonary complications. Methods: This retrospective cohort study included adults undergoing elective open cardiac surgery at our institution from January 2018 through January 2019, who had an American Society of Anesthesiologists score of 3 or greater. For mechanically ventilated patients after cardiac surgery, a new OPE protocol was adopted, comprising an initial 10-min OPE treatment administered in-line with the ventilator circuit, then continued treatments for 48 h after extubation. The primary outcome measure was the occurrence of severe postoperative respiratory complications, including the need for antibiotics, increased use of supplemental oxygen, and prolonged hospital length of stay (LOS). Demographic, clinical, and outcome data were compared between patients receiving usual care (involving post-extubation hyperinflation) and those treated under the new OPE protocol. The primary outcome measure was the occurrence of severe postoperative respiratory complications, including the need for antibiotics, increased use of supplemental oxygen, and prolonged hospital length of stay (LOS). Demographic, clinical, and outcome data were compared between patients receiving usual care (involving post-extubation hyperinflation) and those treated under the new OPE protocol. Results: Of 104 patients, 54 patients received usual care, and 50 received OPE. Usual-care recipients had more men (74% vs. 62%;
p = 0.19) and were older (median, 70 vs. 67 years;
p = 0.009) than OPE recipients. The OPE group had a significantly shorter hospital LOS than the usual-care group (mean, 6.2 vs. 7.4 days;
p = 0.04). Other measures improved with OPE but did not reach significance: shorter ventilator duration (mean, 0.6 vs. 1.1 days with usual care;
p = 0.06) and shorter LOS in the intensive care unit (mean, 2.7 vs. 3.4 days;
p = 0.06). On multivariate analysis, intensive care unit LOS was significantly shorter for the OPE group (mean difference, −0.85 days; 95% CI, −1.65 to −0.06;
p = 0.04). The OPE group had a lower percentage of postoperative complications (10% vs. 20%). Conclusions: OPE therapy after cardiac surgery is associated with decreased intensive care unit (ICU) and hospital LOS.
Full article