Learn more: PMC Disclaimer | PMC Copyright Notice
Resistance Exercise to Prevent and Manage Sarcopenia and Dynapenia
Abstract
For well over twenty centuries the muscle wasting (sarcopenia) and weakness (dynapenia) that occurs with old age has been a predominant concern of mankind. Exercise has long been suggested as a treatment to combat sarcopenia and dynapenia, as it exerts effects on both the nervous and muscular systems that are critical to positive physiological and functional adaptations (e.g., enhanced muscle strength). For more than two decades scientists have recognized the profound role that progressive resistance exercise training can have on increasing muscle strength, muscle size and functional capacity in older adults. In this review article we discuss how resistance exercise training can be used in the management and prevention of sarcopenia and dynapenia. We first provide an overview of the evidence for this notion and highlight certain critical factors— namely exercise intensity, volume and progression— that are key to optimizing the resistance exercise prescription. We then highlight how many, if not most, of the commonly prescribed exercise programs for seniors are not the ‘best practices’, and subsequently present easy-to-read guidelines for a well-rounded resistance exercise training program designed for the management and prevention of sarcopenia and dynapenia, including example training programs for the beginner through the advanced senior resistance exerciser. These guidelines have been written for the academician as well as the student and health care provider across a variety of disciplines, including those in the long term care industry, such as wellness instructors or activity directors.
For well over twenty centuries the muscle wasting and weakness that occurs with old age has been a predominant concern of mankind. As eloquently reviewed by Narici and Maffulli (Narici & Maffulli, 2010), the Classic Greeks (4th and 5th centuries BC) detested the degrading effects of aging on their bodies and considered it a chronic, incurable, and progressive disease. However, by the 1st century BC and the 1st century AD the perspective on physical frailty and aging started to change as Cicero and others began to view aging not as an irreversible illness, but rather a modifiable condition. In fact, in his ‘Essay on Old Age’ in 44 BC Cicero argues that ‘it is our duty… to resist old age, to compensate for its defects, to fight against it as we would fight a disease; to adopt a regimen of health; to practice moderate exercise; and to take just enough food and drink to restore our strength’. While Cicero’s suggestion to use exercise to combat muscle wasting and weakness was logical, it did not truly gain steam in the scientific and medical communities until the latter part of the 20th century. In particular, a series of landmark studies published in the early 1990’s by Fiatarone and colleagues in the Journal of the American Medical Association (Fiatarone et al., 1990) and the New England Journal of Medicine (Fiatarone et al., 1994) highlighted the profound role that progressive resistance exercise training1 (RET) can have on increasing muscle strength, muscle size and functional capacity in older adults. For instance, the first of these studies demonstrated that institutionalized, nonagenarians (i.e., individuals from 90 to 99 years old) were able to increase their muscle strength, on average, an astounding 174%, their mid-thigh muscle area 9.0%, and their gait speed 48% with 8-weeks of high-intensity progressive RET (Fiatarone et al., 1990). By the start of the 21st century we knew that muscle fiber types of older adults were able to hypertrophy (~30% increase in size with 16 weeks of high-intensity RET), transition their fiber type (from type IIX fibers to IIA), and had the capacity to incorporate new nuclei into the fibers (Hikida et al., 2000). These adaptations are comparable to what is observed in younger individuals suggesting that the muscle of older adults is not limited in its ability to adapt. Some two decades later, there is now evidence indicating that high-intensity RET, when coupled with other targeted multidisciplinary interventions, results in lower mortality, nursing home admissions, and disability compared with usual care after hip fracture (Singh et al., 2012).
With the demographic profile of the United States, and the world for that matter, changing (e.g., more than 14% of the entire U.S population is now greater than 65 years (Bureau, 2015)) there is a continued and growing interest in developing effective interventional strategies to combat muscle wasting and weakness associated with aging. To date, the scientific evidence suggests that high-intensity, progressive RET (also commonly referred to as ‘strength training’) is one of, if not the most, effective interventional strategies to enhance muscle size and strength in the elderly (Bird, Hill, Ball, & Williams, 2009; Chale et al., 2013; Charette et al., 1991; Fiatarone et al., 1990; Fiatarone et al., 1994; Hikida et al., 2000; Kalapotharakos, Diamantopoulos, & Tokmakidis, 2010; Liu & Latham, 2009; T. Manini et al., 2007; Sylliaas, Brovold, Wyller, & Bergland, 2011; Van Roie, Delecluse, Coudyzer, Boonen, & Bautmans, 2013). Accordingly, in this article we will briefly review the current literature regarding the use of RET to prevent and manage sarcopenia and dynapenia, and provide pragmatic advice for patients and practitioners on the resistance exercise prescription for older adults. First, however, we will discuss sarcopenia and dynapenia with special attention on their operational definitions.
Sarcopenia is a term, originally proposed by Rosenberg in 1989 (Rosenberg, 1989), specifically referring to the loss of muscle mass associated with ageing. However, the meaning of this term has often been extended to the age-related loss of muscle strength and/or physical function. Although sarcopenia is certainly a contributor to muscle weakness, it has been argued that these two terms should not be used interchangeably since this would imply a direct proportionality between the two (Clark & Manini, 2008; T. M. Manini & Clark, 2011; T.M. Manini, Russ, & Clark, 2012; Narici & Maffulli, 2010; Visser & Schaap, 2011), which is not the case as a variety of other neural and muscular factors contribute to force output that are independent of muscle mass (For review see: (Clark & Manini, 2008; Duchateau & Enoka, 2002; T. M. Manini & Clark, 2011; T.M. Manini et al., 2012; Narici & Maffulli, 2010)). Accordingly, the term dynapenia was proposed by Clark and Manini in 2008 to specifically refer to the loss of muscle strength and power associated with aging (Clark & Manini, 2008).
While there are semantic debates in the literature, there is progress towards developing criteria/criterion for the diagnosis of clinically significant sarcopenia and/or dynapenia in recent years. For example, the European Working Group on Sarcopenia in Older People incorporates aspects of 1) physical function (i.e., gait speed), 2) muscle strength, and 3) muscle mass into a singular diagnosis of sarcopenia (Cruz-Jentoft et al., 2010). Other criteria, namely those by the Foundation for the National Institutes of Health’s Sarcopenia Working Group, attempted to define low muscle mass and muscle weakness independently using a data driven approach in a pooled sample of 26,635 older adults (Studenski et al., 2014). While there are significant efforts being put forth by both researchers and practitioners in the development of diagnostic criteria, it is important to note there are no established agreed upon definition for these common conditions at this time.
RET and the Management and Prevention of Muscle Wasting and Weakness
While sarcopenia and dynapenia are realized to be major clinical problems for older adults, until recently there has been little wide spread support for ways to combat these debilitating conditions. However, research on the effects of exercise and nutrition on sarcopenia and dynapenia has rapidly expanded in the past one to two decades (Sayer et al., 2013). Today, there is still limited evidence suggesting that pharmacologic interventions effectively ameliorate sarcopenia and/or dynapenia. However, there is strong and growing evidence that progressive RET can combat both sarcopenia and dynapenia (Burton & Sumukadas, 2010), as RET has a profound effect on virtually all of the physiological mechanisms in the nervous system and the muscular system known to influence strength (Duchateau & Enoka, 2002; Russ, Gregg-Cornell, Conaway, & Clark, 2012). For instance, maximal motor unit discharge rates, a key ‘neural factor’ involved in muscle strength, increased 49% in older adults following only 6-weeks of high-intensity progressive RET (Kamen & Knight, 2004). Non-mass dependent muscular factors, such as muscle fiber fascicle length and tendon stiffness, have also been observed to increase (10% and 64%, respectively) following RET in older adults 64%, respectively (Reeves, Maganaris, & Narici, 2003). Additionally, RET is also a powerful stimulus for inducing muscle hypertrophy as illustrated by 24-weeks of RET, when coupled with modest protein supplementation, increasing thigh muscle cross-sectional area 4.6% in mobility limited older adults (Chale et al., 2013). Given that there exists widespread evidence that inactivity, which is prevalent in the elderly (Troiano et al., 2008), leads to loss of muscle mass and strength (Clark, 2009), findings of this nature would (or should) lead all scientists and clinicians to support the use of RET for treating, slowing, and/or preventing sarcopenia and dynapenia.
Indeed, the extant literature supports this notion. For instance, a 2009 Cochrane review of 121 trials including over 6,700 participants concluded that ‘progressive resistance training is an effective intervention for improving physical functioning in older people, including improving strength and the performance of some simple and complex activities’ (Liu & Latham, 2009). Most of the trials reviewed involved high intensity training two to three times per week. Benefits included large positive effects on both muscle mass (hypertrophy) and strength (Liu & Latham, 2009). A functional assessment of gait speed showed a modest improvement and a strong effect was observed on the ability to rise from a chair (Liu & Latham, 2009).
It is well recognized that the effectiveness of RET for strength and muscle mass improvement is variable across studies, and recent meta-analyses by Peterson and colleagues attempted to identify critical aspects of RET programs which promote strength adaptation (e.g., the frequency of exercise training, the duration of exercise training, the intensity of exercise training, the volume of exercise training, etc.) (Peterson, Rhea, Sen, & Gordon, 2010; Peterson, Sen, & Gordon, 2011). These studies revealed two critical aspects for positive adaptations associated with progressive RET. First, higher intensity RET is associated with greater improvements in muscle strength. Specifically, with each incremental increase in exercise intensity from low intensity (<60% of 1-repetition maximum or 1-RM), low/moderate intensity (60–69% of 1-RM), moderate/high intensity (70–79% of 1-RM) to high-intensity (≥80% of 1-RM) the average percent change in strength was 5.3% (Figure 1A) (Peterson et al., 2010). Second, higher RET volume, defined as the total number of exercise sets performed per session, is associated with greater improvements in lean body mass after controlling for a variety of confounders (e.g., age, study duration, gender, training intensity and frequency, etc.) (Figure 1B) (Peterson et al., 2011). This finding suggests that for every additional 10 sets of exercise performed per session that one can expect, on average a 0.5 kg increase in lean body mass (Peterson et al., 2011). It should be noted that this study reported the older individuals experienced a lesser increase in LBM with RET (Peterson et al., 2011). Some scientists have suggested that there are “non-responders” to progressive RET (Bamman, Petrella, Kim, Mayhew, & Cross, 2007); however, a recent retrospective analysis revealed that, while there is a large heterogeneity in the adaptive response to prolonged RET as it relates to changes in strength and mass, the level of responsiveness was strongly affected by the duration of the exercise intervention, with more positive responses following more prolonged exercise training (Churchward-Venne et al., 2015). Accordingly, these findings suggest that there are no true “non-responders” to the benefits of RET amongst the elderly and that it should be promoted without restriction to prevent and manage sarcopenia and dynapenia. In figure 2 we present conceptual interactions between physical activity, sarcopenia, dynapenia, fatigability, exercise tolerance, and physical function (Figure 2A) and how progressive resistance exercise training can modulate these various phenotypic factors (Figure 2B).
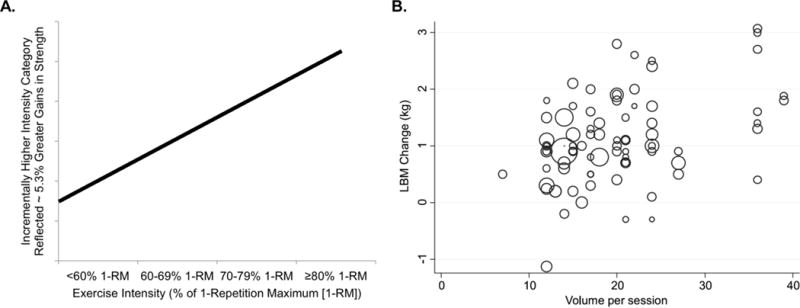
Figure 1A: Peterson et al. reported in a meta-analysis that with each incremental increase in exercise intensity from low intensity (<60% of 1-RM), low/moderate intensity (60–69% of 1-RM), moderate/high intensity (70–79% of 1-RM) to high-intensity (≥80% of 1-RM) training the average percent change in strength was 5.3% (Peterson et al., 2010). Figure 1B: LBM change by training volume (defined as sets per session) when weighted by the number of subjects in a given study using a meta analytical approach (Peterson et al., 2011).
Figure 1A was created from data presented in Peterson et al., Resistance exercise for muscular strength in older adults: a meta-analysis. Ageing Research Reviews, 226–237, 2010. Figure 1B was reprinted with permission by Peterson et al., Influence of resistance exercise on lean body mass in aging adults: a meta-analysis. Med Sci Sports Exerc, 43: 249–258, 2011.
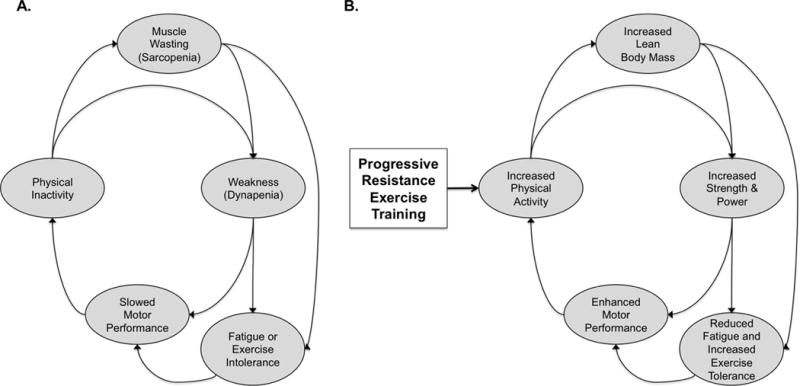
Note that other influences, such as nutritional, cognitive, and psychological factors, are not shown for clarity.
Adapted with permission from Liu and Fielding. Exercise as an intervention for frailty. Clin Geriatr Med. 27:101–10, 2011.
The Common Practices Are Not the Best Practices
Unfortunately, many older people are unable or unwilling to embark on strenuous exercise training programs, and, despite a call from the American Academy of Family Physicians (Physicians, 2015), many seniors are often prescribed “low dose” resistance exercise programs that are physiologically inadequate to increase gains in muscle mass and strength. In 2004, the National Council on Aging (NCOA) Center for Healthy Aging released a guide entitled “Best Practices in Physical Activity” in order to disseminate information to the public regarding the best-practice and evidence-based models which were being employed at a community level (local public or non-profit organizations) to facilitate older adults in achieving and maintaining functional independence and vitality (NCOA, 2004). A team of experts developed best-practice criteria based on expert opinion and findings from the literature and identified 10 community-based programs as national best-practice programs. In 2009, Hughes et al. assessed the impact of these 10 best-practice physical activity programs for older adults in terms of health related outcomes (Hughes, Seymour, Campbell, Whitelaw, & Bazzarre, 2009). Not surprisingly, these community-based physical activity programs, which utilized multiple-component physical activity interventions, measurably improved aspects of physical function that are risk factors for disability among older adults. Unfortunately, our anecdotal observation is that there is a large degree of variability in the implementation of physical activity programs in the community-based setting. Common barriers to implementation and participation in community-based exercise programs are program costs, lack of transportation/accessibility, lack of necessary time commitment, unsupportive physical environments, psychological barriers with regards to negative connotations of exercising in the older adults, as well as lack of expertise (Mathews et al., 2010, Boyette et al., 2002, Schutzer et al., 2004). In 2009, Cress et al. identified the key components of best practice physical activity programs for older adult populations as being 1) muscular strength and endurance, 2) balance, 3) cardiovascular endurance, and 4) flexibility (Cress et al., 2005). While many of the existing best practice community programs incorporate these components into their physical activity interventions, very few have adopted the American College of Sports Medicine (ACSM) guidelines for progressive high intensity RET to promote muscle hypertrophy, strength and power (American College of Sports, 2009). An example of one such program is the National Institute on Aging’s Go4Life program (NIA, 2015). While this program encourages older adults to create personal physical activity programs incorporating all four of these key components, the examples provided for muscular strength training/resistance exercises on the Go4Life website are very low to moderate intensity exercises for most seniors and are difficult to progress as they utilize wrist weights, TheraBand™, small hand weights, and gravity-reduced body weight resistance exercises. Similarly, our observations indicate that many rehabilitation facilities (including hospitals, short-term and long-term stay facilities) have not adopted high-intensity progressive RET into their standard protocol for the pre-frail and frail elderly client/patient populations. While many of these facilities offer 60 minutes of therapy twice per day, they commonly use low intensity exercise (e.g., seated in a wheelchair performing knee extension exercises with ankle weights) in conjunction with some functional training (i.e., wheelchair transfers), and aerobic activity. While the types of exercises mentioned above present adequate entry-level exercises for seniors, they are not likely a sufficient stimulus to promote positive muscle growth and adaptation. Accordingly, in the following section we attempt to provide pragmatic resistance exercise advice for patients and practitioners.
Pragmatic Resistance Exercise Advice for Patients and the Practitioner
When developing RET programs for older adults it is important to consider all of the various training-related variables, such as, frequency, duration, exercises, sets, intensity, repetitions, and progression. Also, many older adults often have existing health issues (e.g., orthopedic limitations, cardiovascular disease, etc.) that require special consideration. The Exercise And Screening for You (EASY) survey is a tool that helps provide guidance on appropriate exercise programs for seniors (Program on Healthy Aging, 2008). It is also suggested that older adults who are beginning a RET program receive proper instruction and supervision by an appropriately trained exercise professional, such as a physical therapist or an exercise physiologist.
RET Frequency
Exercise frequency refers to the number of exercise sessions per week. With regards to older adults performing RET, two to four days per week are commonly recommended with training typically being performed on alternating days (e.g., Monday, Wednesday and Friday) (Willoughby, 2015). The most common approach for someone beginning a RET program is to perform a ‘total body’ exercise routine whereby all of the major muscle groups are exercised at each exercise session with the ‘total body’ routine being performed 2–3 times per week. An alternative approach, which is more commonly used in more advanced RET programs involves exercising selected muscle groups on one or two days per week while the remaining are exercised on a separate one or two days per week (e.g., chest, back and upper legs on Monday; arms, shoulders, and lower legs on Tuesday; chest, back and upper legs on Thursday; arms, shoulders, and lower legs on Friday).
RET Duration
Duration describes the length of each training session. The total duration of RET programs are highly variable and not commonly studied per se as there are many extraneous factors that contribute to duration (e.g., rest time between sets). In general, however, most RET sessions should be able to be completed in 30-minutes to an hour (at an advanced level more time may be required). The amount of rest taken between sets is a highly influential variable that affects the total duration (alongside the number of sets, exercises, etc.). With respect to between set rest interval, the American College of Sports Medicine currently recommends 1–2 min rest intervals for training programs designed to stimulate muscular hypertrophy in novice and intermediate healthy resistance exercisers (American College of Sports, 2009). With this said, many authors have proposed that rest intervals of 30–60 seconds are optimal because they result in the greatest exercise-induced elevations in selected anabolic hormones, notably growth hormone (de Salles et al., 2009; Willardson, 2006). The current literature does not support this notion per se (Henselmans & Schoenfeld, 2014); however, many experienced practitioners anecdotally report more hypertrophic gains with shorter rest intervals.
RET Exercises
Exercises are commonly categorized as either multi-joint or uni-joint. Multi-joint exercises are those in which more than one joint is involved in the exercise, such as the chest press and leg press. Uni-joint exercises are those where only one joint is involved, such as bicep curls and leg extensions). For older adults, multi-joint exercises should be encouraged (due to their functional relevance) (Willoughby, 2015), although uni-joint exercises should not necessarily be discouraged. Additionally, resistance exercise machines (e.g., leg press machines) are recommended for the beginner over free weights (i.e., barbells and dumbbells) as less skill is required when using machines, and the movement restrictions of the machines provide greater safety for the user. As an individual progresses; however, free-weight exercises appropriate for level of skill, training status and functional capacity is reasonable.
The specific exercises to perform can be highly variable depending on the availability of equipment, but a well-rounded RET program should include exercises that involve all of the “major muscle groups”. These muscle groups are commonly defined as the chest, back, arms, shoulders, upper legs (quadriceps, hamstrings, and gluteals), and lower legs (calves). Examples of different exercises for each of these major muscle groups are provided in Table 1. One to two exercises per muscle group is adequate for the beginner and intermediate (Willoughby, 2015), and it should be noted that performing multi-joint exercises results in multiple muscle groups being exercised (e.g., chest press exercises not only the chest (pectoralis) muscles, but also the triceps and the anterior compartment of the shoulder). In general, it is recommended that multi-joint exercises be performed before uni-joint exercises for a particular muscle group, and that within each session the larger muscle groups be exercised before the smaller muscle groups (Willoughby, 2015).
Table 1
Example exercises for the major muscle groups.
| Muscle Group | Exercises |
|---|---|
| Chest | Flat Chest Press (Machine*, Barbell**, or Dumbbell**) |
| Chest Flyes (Machine*, Flat dumbbell flyes**, incline or decline flyes***) | |
| Incline or Decline Chest Press (Machine**, Barbell***, or Dumbbell***) | |
| Push-Ups (Modified with knees on ground** or unmodified with feet on ground***) | |
| Back | Pull Downs or Seated Cable Rows (Machine*) |
| Chest Supported Rows (Machine**, Barbell***, Dumbbell***) | |
| Pull-Ups (with machine body weight assist** or no body weight assist***) | |
| Shrugs (Machine**, Barbell***, Dumbbell***) | |
| Arms | Seated Curls (Machine*, Barbell**, or Dumbbell**) |
| Hammer or Preacher Curls (Dumbbell**) | |
| Triceps Extension (Machine*, Cable Press-Down*, or Prone Barbell or Dumbbell***) | |
| Bent Over Triceps Extension ‘Kick Backs’ (Dumbbell**) | |
| Shoulders | Overhead Press (Machine*, Barbell***, or Dumbbell***) |
| Upright Rows (Machine**, Barbell***, or Dumbbell***) | |
| Lateral Raises (Machine*, Barbell***, or Cable***) | |
| Rear Deltoid Rows/Flyes (Machine**, Barbell***, or Dumbbell***) | |
| Upper Legs | Leg Press (Machine*) |
| Leg Extensions (quadriceps) and Curls (hamstrings) (Machine*) | |
| Lunges (No weight**, Barbell***, or Dumbbell***) | |
| Machine Squat*** | |
| Lower Legs | Standing Calf Raises (No weights*, with additional weight via machine or dumbbells***) |
| Seated Calf Raises (Machine*) |
Exercises denoted with an asterisk* are recommended for the beginner. Exercises noted with two asterisks** are recommended for an intermediate level, and exercises noted with three asterisks*** are only recommended for an advanced level. Resistance exercise machines are recommended for the beginner over free weights. As an individual progresses; however, free-weight exercises appropriate for level of skill, training status and functional capacity is reasonable. Additionally, multi-joint exercises are recommended as these frequently have higher functional relevance and also result in more than one muscle group being exercised.
RET Sets
Significant improvements in muscle strength and size have been observed with the number of sets ranging between one to three (Starkey et al., 1996). We recommend that an individual start with a familiarization period that lasts 1–2 weeks where one set of each exercise is performed with heavy emphasis placed on safety and form. Next, depending on individual need, progression up to three sets in the beginner phase is reasonable when deemed appropriate. With progression to an intermediate and advanced stage, additional sets or additional exercises can be added to increase the overall volume of training (total number of sets per session), which, as illustrated in Figure 2B is critical for hypertrophic gains. Also, as mentioned previously, the inter-set rest interval is important to consider, and sufficient rest should be taken to avoid excessive fatigue (i.e., enough rest so that the remaining sets can be performed with the appropriate form), but an excessively long rest period should be avoided.
RET Intensity
Intensity refers to the relative amount of weight being lifted (i.e., the percentage of maximum). As illustrated in Figure 1A the RET intensity is a critical factor in determining the amount of neuromuscular adaptation induced via training. Numerous studies have now illustrated that high-intensity RET (e.g., 80+% of 1-RM) is tolerated in older adults (Chale et al., 2013; Fiatarone et al., 1994 ; Reeves et al., 2003; Singh et al., 2012). Accordingly, we suggest that RET intensity should be progressed to the “high-intensity” as permitted. However, it should be noted that studies have shown intensities ranging from 65%–75% of maximum will increase strength, and some authors suggest these intensities should be utilized as an attempt to decrease the risk of musculoskeletal injury (Willoughby, 2015).
RET Repetitions
Repetitions refer to the number of times an individual performs a complete movement of a given exercise. The number of repetitions that one can perform is inversely related to the exercise intensity (i.e., the higher the intensity the fewer repetitions that can be performed). As illustrated in Figure 3, if an individual is exercising at 60% of his/her maximum strength, he/she will likely be able to perform between 18–32 repetitions to “task failure” using free weights. At 80% of the individual’s maximum strength, the number of repetitions to failure is generally between 8–15, and at 90% it is 4–12 repetitions with free weights. The number of repetitions to failure for machines is, generally speaking, slightly higher than with free weights (Figure 3) presumably due to free weights requiring more muscles for stabilization and balance compared to a fixed path machine lifting task. Understanding these relationships is important, as it provides a mechanism for a trial-and-error approach to be utilized to prescribe the appropriate training load without having to actually test muscle strength (e.g., performing the exercise to task failure within 10–15 repetitions would likely indicate that an individual is exercising at an intensity in the 70–85% of maximum strength range).
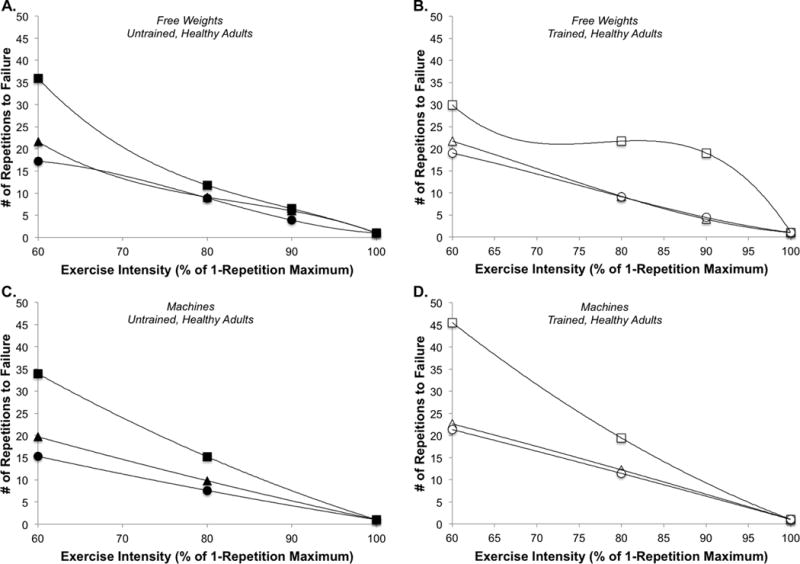
Relationship between the number of repetitions untrained (3A) and trained (3B) healthy adults were able to perform using free weights at four different resistance exercise intensities (60, 80 and 90% of 1-RM) for the squat (square), bench press (triangle), and arm curl (circle). Relationship between the number of repetitions untrained (3C) and trained (3D) healthy adults were able to perform using resistance exercise machines at three different resistance exercise intensities (60, 80 and 1-RM) for the leg press (square), chest press (triangle), and arm curl (circle). Data represents the mean response for each exercise and intensity, respectively.
Figure 3A and 3B created from data presented in Shimano et al., Relationship between the number of repetitions and selected percentages of one repetition maximum in free weight exercises in trained and untrained men. J Strength and Conditioning Research. 20: 819–823, 2006.
Figure 3C and 3D created from data presented in Hoeger et al., Relationship between repetitions and selected percentages of one repetition maximum: a comparison between untrained and trained males and females. J Applied Sport Science Research. 4: 47–54, 1990.
RET Progression
The concept of “progression” refers to gradually overloading, or increasing the stress, placed on the body during exercise. The human body will only respond if it is continually required to exert a greater magnitude of force (or higher volume) to meet higher physiological demands. Thus, in order to continually enjoy improvements in mass, strength and functional capacity, it is important to consistently incorporate progression and variation into the RET program. There are an ample number of ways to progress a RET program. For instance, one can make adjustments by increasing the frequency, duration, exercises performed, number of exercises for each muscle group, sets and repetitions. Progression should be a gradual process with adjustments made on a monthly basis commonly recommended (Willoughby, 2015). During progression it is important for the exercise professional to be aware of the patients medical limitations and for progression to occur via adjustments in the most appropriate training variables on a case-by-case basis.
In Tables 2–5 we present an example progressive RET program. This program is designed for an older adult without any contraindications for RET training. Modifications would need to be made if certain musculoskeletal, neurological, or mobility limitations precluded an individual from safely performing the program. This program is designed on the assumption that access to typical machine and free weight resistance exercise equipment is available, but it could be modified as needed based on equipment availability. Additionally, progression could be varied (sped up or slowed down) depending on individual adaptation.
Table 2
It is suggested that the exercise is performed to, or near, task failure in the range of repetitions provided.
| Beginner: Phase I | ||
|---|---|---|
| 50–60% of 1-RM; 2×/week | 1–2 Weeks; Familiarization Phase | |
|
| ||
| Body Part | Exercise | Sets × Reps |
|
| ||
| Chest | Chest Press (Machine: seated or lying) | 1 × 15–12 |
|
| ||
| Back | Seated Cable Row | 1 × 15–12 |
| Seated Cable Pull Down | 1 × 15–12 | |
|
| ||
| Arms | Biceps Curl (Seated Machine) | 1 × 15–12 |
| Triceps Extension (Seated Machine) | 1 × 15–12 | |
|
| ||
| Shoulders | Overhead Press (Seated Machine) | 1 × 15–12 |
|
| ||
| Upper Legs | Leg Extensions (Seated Machine) | 1 × 15–12 |
| Leg Curl (Seated Machine) | 1 × 15–12 | |
|
| ||
| Lower Legs | Calf Raise (Seated Machine) | 1 × 15–12 |
| Calf Raise (Standing) | 1 × 15–12 | |
|
| ||
| Rest Between Sets: 2 minutes (as needed) | Total Sets: 10 | |
| Beginner: Phase II | ||
|---|---|---|
| 60–69% of 1-RM; 2×/week | 3–8 Weeks | |
|
| ||
| Body Part | Exercise | Sets × Reps |
|
| ||
| Chest | Chest Press (Machine: seated or lying) | 1 × 12–18 |
| Wall Push-Ups | 1 × 12–18 | |
|
| ||
| Back | Seated Cable Row | 1 × 12–18 |
| Seated Cable Pull Down | 1 × 12–18 | |
|
| ||
| Arms | Biceps Curl (Seated Machine) | 1 × 12–18 |
| Triceps Extension (Seated Machine) | 1 × 12–18 | |
|
| ||
| Shoulders | Overhead Press (Seated Machine) | 1 × 12–18 |
|
| ||
| Upper Legs | Leg Extensions (Seated Machine) | 1 × 12–18 |
| Leg Curl (Seated Machine) | 1 × 12–18 | |
|
| ||
| Lower Legs | Calf Raise (Seated Machine) | 1 × 12–18 |
| Calf Raise (Standing) | 1 × 12–18 | |
|
| ||
| Rest Between Sets: 90 seconds | Total Sets: 11 | |
Table 5
It is suggested that the exercise is performed to, or near, task failure in the range of repetitions provided.
| Advanced: Phase II | ||
|---|---|---|
| >80% of 1-RM; 4×/week Split | 32+ Weeks | |
|
| ||
| Body Part | Exercise | Sets × Reps |
|
| ||
| MONDAY & THURSDAY | ||
|
| ||
| Chest | Chest Press (Barbell or Dumbbell) | 3 × 6–10 |
| Incline or Decline Chest Press (Barbell or Dumbbell) | 3 × 6–10 | |
| Chest Flyes (Lying with dumbbells) | 3 × 6–10 | |
| Push-Ups | 3 × 6–10 | |
|
| ||
| Back | Chest Supported Rows (Barbell or Dumbbell) | 3 × 6–10 |
| Pull Ups (With or without assist) | 3 × 6–10 | |
| Shoulder Shrugs (Barbell or Dumbbell) | 3 × 6–10 | |
|
| ||
| Upper Legs | Squat (Machine) | 3 × 6–10 |
| Leg Extensions (Seated Machine) | 3 × 6–10 | |
| Leg Curl (Seated Machine) | 3 × 6–10 | |
| Lunges (Dumbbell) | 3 × 6–10 | |
|
| ||
| TUESDAY & FRIDAY | ||
|
| ||
| Arms | Biceps Curl (Standing Barbell) | 3 × 6–10 |
| Biceps Curl (Seated Dumbbell) | 3 × 6–10 | |
| Hammer or Preacher Curls (Seated Dumbbell) | 3 × 6–10 | |
| Triceps Extension (Lying with Barbell or Dumbbell) | 3 × 6–10 | |
| Triceps Kick Backs (Dumbbells) | 3 × 6–10 | |
|
| ||
| Shoulders | Overhead Press (Barbell or Dumbbell) | 3 × 6–10 |
| Lateral Raises (Dumbbell or Cable) | 3 × 6–10 | |
| Rear Deltoid Flyes (Machine or Dumbbells) | 3 × 6–10 | |
| Upright Rows (Barbell or Dumbbells) | 3 × 6–10 | |
|
| ||
| Lower Legs | Calf Raise (Seated Machine) | 3 × 6–10 |
| Calf Raise (Standing) | 3 × 6–10 | |
|
| ||
| Rest Between Sets: 60 seconds | Total Sets: 33 sets/day | |
Exercise Program Modifications
There are a certainly individuals who will not be able to perform the type of RET program as described due to limited access to exercise equipment or fitness facilities. However, there are a variety of approaches that can successfully be used to overcome these limitations. For instance, task specific, functional exercises can be performed. Additionally, many of the exercises in our example RET program can be completed using only limited equipment. These kinds of modifications essentially result in more of a “free weight” style exercise program and, as such, special care should be taken to pay close attention to using proper exercise form.
Additionally, “functional” or “task specific” exercise has merit for enhancing physical function in older adults. An article published by Manini, and colleagues (2007) provided evidence that functional, task specific training reduces the need for task modification for activities of daily living in seniors who report regularly modifying tasks of daily life, but who are not yet disabled (T. Manini et al., 2007). This type of training involved performing specific functional tasks, which are activities of everyday life, such as standing up from a chair, lifting and carrying a loaded laundry basket, vacuuming, or even ascending and descending a flight of stairs. The principles of overload and resistance progression can conceptually be applied to functional tasks as well. For example, an effective functional quadriceps and gluteal exercise that mimics a leg press exercise is standing up from a chair. A low intensity version of this exercise is to stand up from a chair for a given number of repetitions with the arms across the chest. One can increase the intensity by reducing the seat pan height, altering the movement velocity (performing either slower, more controlled movements or by performing faster, more powerful movements), and/or performing the task while holding or wearing additional weight (T. Manini et al., 2007). An example of an upper extremity functional exercise is lifting and carrying household items (e.g., a bag of groceries) and placing it on a shelf. One can increase the intensity by altering the height it is lifted, the distance carried, and/or the amount of weight being lifted and carried.
The exercises that are suggested in Tables 2–5 can also be adapted for use at home with just a few dumbbells, household items (e.g., milk jug) and elastic bands (e.g., Therabands®). For instance, instead of the leg press exercises, one can perform squats initially by using only the resistance of his/her own body weight, but then increasing the resistance by holding a half filled milk jug in either hand. A higher intensity version of this exercise would be to complete 2 to 3 sets of a given number of repetitions while holding milk jugs filled to capacity in each hand. Similarly, substituting a single arm row using some type of free weight (e.g., a dumbbell or a household item) can serve as an effective exercise stimulus for the back musculature. In essence, there are many ways to be creative with exercise programming outside of a fitness facility environment; however, one must keep in mind that in the absence of a trained fitness instructor in the home environment, coupled with performing exercises where movement is more unconstrained, that proper lifting technique must be established and followed in order to prevent injury.
Conclusions
A well-designed, progressive resistance exercise training program is well known to exert positive effects on both the nervous and muscular systems and, ultimately, results in profound enhancements in muscle mass and muscle strength. Accordingly, resistance exercise training should be considered a first-line treatment strategy for managing and preventing both sarcopenia and dynapenia. While there are many components to an optimal resistance exercise prescription, exercise intensity, exercise volume and progression, are critical factors that deserve strong consideration as it relates to following best practice guidelines. We hope the example resistance exercise training program presented herein is useful for academicians, students, and health care providers across a variety of disciplines, including those in the long term care industry.
Table 3
It is suggested that the exercise is performed to, or near, task failure in the range of repetitions provided.
| Intermediate: Phase I | ||
|---|---|---|
| 60–69% of 1-RM; 2×/week | 9–16 Weeks | |
|
| ||
| Body Part | Exercise | Sets × Reps |
|
| ||
| Chest | Chest Press (Machine: seated or lying) | 2 × 12–18 |
| Wall Push-Ups | 2 × 12–18 | |
| Chest Flyes (Machine) | 2 × 12–18 | |
|
| ||
| Back | Seated Cable Row | 2 × 12–18 |
| Seated Cable Pull Down | 2 × 12–18 | |
|
| ||
| Arms | Biceps Curl (Seated Machine) | 2 × 12–18 |
| Triceps Extension (Seated Machine) | 2 × 12–18 | |
|
| ||
| Shoulders | Overhead Press (Seated Machine) | 2 × 12–18 |
| Lateral Raises (Seated Machine) | 2 × 12–18 | |
|
| ||
| Upper Legs | Leg Press (Machine) | 2 × 12–18 |
| Leg Extensions (Seated Machine) | 2 × 12–18 | |
| Leg Curl (Seated Machine) | 2 × 12–18 | |
|
| ||
| Lower Legs | Calf Raise (Seated Machine) | 2 × 12–18 |
| Calf Raise (Standing) | 2 × 12–18 | |
|
| ||
| Rest Between Sets: 90 seconds | Total Sets: 28 | |
| Intermediate: Phase II | ||
|---|---|---|
| 70–79% of 1-RM; 3×/week | 17–24 Weeks | |
|
| ||
| Body Part | Exercise | Sets × Reps |
|
| ||
| Chest | Chest Press (Barbell) | 2 × 10–15 |
| Chest Flyes (Lying with dumbbells) | 2 × 10–15 | |
| Push-Ups (Knees down) | 2 × 10–15 | |
|
| ||
| Back | Chest Supported Rows (Machine) | 2 × 10–15 |
| Pull Ups (Machine with body weight assist) | 2 × 10–15 | |
|
| ||
| Arms | Biceps Curl (Seated Dumbbell) | 2 × 10–15 |
| Triceps Extension (Cable Press Down) | 2 × 10–15 | |
| Triceps Kick Backs (Dumbbells) | 2 × 10–15 | |
|
| ||
| Shoulders | Overhead Press (Seated Machine) | 2 × 10–15 |
| Lateral Raises (Seated Machine) | 2 × 10–15 | |
| Upright Rows (Barbell or Dumbbells) | 2 × 10–15 | |
|
| ||
| Upper Legs | Leg Press (Machine) | 2 × 10–15 |
| Leg Extensions (Seated Machine) | 2 × 10–15 | |
| Lunges (No Weight) | 2 × 10–15 | |
| Leg Curl (Seated Machine) | 2 × 10–15 | |
|
| ||
| Lower Legs | Calf Raise (Seated Machine) | 2 × 10–15 |
| Calf Raise (Standing) | 2 × 10–15 | |
|
| ||
| Rest Between Sets: 90 seconds | Total Sets: 34 | |
Table 4
It is suggested that the exercise is performed to, or near, task failure in the range of repetitions provided.
| Advanced: Phase I | ||
|---|---|---|
| >80% of 1-RM; 3×/week | 25–32 Weeks | |
|
| ||
| Body Part | Exercise | Sets × Reps |
|
| ||
| Chest | Chest Press (Barbell) | 2 × 8–12 |
| Chest Flyes (Lying with dumbbells) | 2 × 8–12 | |
| Incline Chest Press (Machine) | 2 × 8–12 | |
| Push-Ups (Knees Down) | 2 × 8–12 | |
|
| ||
| Back | Chest Supported Rows (Machine) | 2 × 8–12 |
| Pull Ups (Machine with body weight assist) | 2 × 8–12 | |
| Shoulder Shrugs (Machine) | 2 × 8–12 | |
|
| ||
| Arms | Biceps Curl (Seated Dumbbell) | 2 × 8–12 |
| Hammer Curls (Seated Dumbbell) | 2 × 8–12 | |
| Triceps Extension (Cable Press Down) | 2 × 8–12 | |
| Triceps Kick Backs (Dumbbells) | 2 × 8–12 | |
|
| ||
| Shoulders | Overhead Press (Seated Machine) | 2 × 8–12 |
| Lateral Raises (Seated Machine) | 2 × 8–12 | |
| Rear Deltoid Flyes (Machine or Dumbbells) | 2 × 8–12 | |
| Upright Rows (Barbell or Dumbbells) | 2 × 8–12 | |
|
| ||
| Upper Legs | Leg Press (Machine) | 2 × 8–12 |
| Leg Extensions (Seated Machine) | 2 × 8–12 | |
| Lunges (No Weight) | 2 × 8–12 | |
| Leg Curl (Seated Machine) | 2 × 8–12 | |
|
| ||
| Lower Legs | Calf Raise (Seated Machine) | 2 × 8–12 |
| Calf Raise (Standing) | 2 × 8–12 | |
|
| ||
| Rest Between Sets: 60–90 seconds | Total Sets: 42 | |
Acknowledgments
We would like to thank Robert S. Staron, Ph.D. (Ohio University) for his thoughtful critique and input on a draft of this manuscript.
Funding: This work was supported in part by the following grants from the National Institutes of Health (NIH) to BC Clark: R01AG044424 from the National Institute on Aging, R01AT006978 from the National Center for Complimentary and Integrative Health, and R21AR063909 from the National Institute for Arthritis and Musculoskeletal and Skin Diseases.
Footnotes
1Progressive RET involves increasing the number of repetitions at a constant load until exceeding an established repetition range (e.g., 12 repetitions). Subsequently, the load is increased and the exercise is performed at the new load until again exceeding the repetition range.
References
- American College of Sports, Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687–708. doi: 10.1249/MSS.0b013e3181915670. [PubMed] [CrossRef] [Google Scholar]
- Bamman MM, Petrella JK, Kim JS, Mayhew DL, Cross JM. Cluster analysis tests the importance of myogenic gene expression during myofiber hypertrophy in humans. J Appl Physiol (1985) 2007;102(6):2232–2239. doi: 10.1152/japplphysiol.00024.2007. [PubMed] [CrossRef] [Google Scholar]
- Bird ML, Hill K, Ball M, Williams AD. Effects of resistance- and flexibility-exercise interventions on balance and related measures in older adults. J Aging Phys Act. 2009;17(4):444–454. [PubMed] [Google Scholar]
- Bureau, US Census. USA Quick Facts from the US Census Bureau. 2015 Retrieved March 23, 2015, 2015, from http://quickfacts.census.gov/qfd/states/00000.html.
- Burton LA, Sumukadas D. Optimal management of sarcopenia. Clin Interv Aging. 2010;5:217–228. [PMC free article] [PubMed] [Google Scholar]
- Chale A, Cloutier GJ, Hau C, Phillips EM, Dallal GE, Fielding RA. Efficacy of whey protein supplementation on resistance exercise-induced changes in lean mass, muscle strength, and physical function in mobility-limited older adults. J Gerontol A Biol Sci Med Sci. 2013;68(6):682–690. doi: 10.1093/gerona/gls221. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Charette SL, McEvoy L, Pyka G, Snow-Harter C, Guido D, Wiswell RA, Marcus R. Muscle hypertrophy response to resistance training in older women. J Appl Physiol (1985) 1991;70(5):1912–1916. [PubMed] [Google Scholar]
- Churchward-Venne TA, Tieland M, Verdijk LB, Leenders M, Dirks ML, de Groot LC, van Loon LJ. There Are No Nonresponders to Resistance-Type Exercise Training in Older Men and Women. J Am Med Dir Assoc. 2015 doi: 10.1016/j.jamda.2015.01.071. [PubMed] [CrossRef] [Google Scholar]
- Clark BC. In Vivo Alterations in Skeletal Muscle Form and Function after Disuse Atrophy. Med Sci Sports Exerc. 2009 doi: 10.1249/MSS.0b013e3181a645a6. [PubMed] [CrossRef] [Google Scholar]
- Clark BC, Manini TM. Sarcopenia =/= dynapenia. J Gerontol A Biol Sci Med Sci. 2008;63(8):829–834. doi: 63/8/829 [pii] [PubMed] [Google Scholar]
- Cress ME, Buchner DM, Prohaska T, Rimmer J, Brown M, Macera C, Chodzko-Zajko W. Best practices for physical activity programs and behavior counseling in older adult populations. J Aging Phys Act. 2005;13(1):61–74. [PubMed] [Google Scholar]
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Zamboni M. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–423. afq034 [pii] 10.1093/ageing/afq034. [PMC free article] [PubMed] [Google Scholar]
- de Salles BF, Simao R, Miranda F, Novaes Jda S, Lemos A, Willardson JM. Rest interval between sets in strength training. Sports Med. 2009;39(9):765–777. doi: 10.2165/11315230-000000000-00000. [PubMed] [CrossRef] [Google Scholar]
- Duchateau J, Enoka RM. Neural adaptations with chronic activity patterns in able-bodied humans. American journal of physical medicine & rehabilitation/Association of Academic Physiatrists. 2002;81(11 Suppl):S17–27. doi: 10.1097/01.PHM.0000029724.14558.BC. [PubMed] [CrossRef] [Google Scholar]
- Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263(22):3029–3034. [PubMed] [Google Scholar]
- Fiatarone MA, O’Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, Evans WJ. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330(25):1769–1775. doi: 10.1056/NEJM199406233302501. [PubMed] [CrossRef] [Google Scholar]
- Henselmans M, Schoenfeld BJ. The effect of inter-set rest intervals on resistance exercise-induced muscle hypertrophy. Sports Med. 2014;44(12):1635–1643. doi: 10.1007/s40279-014-0228-0. [PubMed] [CrossRef] [Google Scholar]
- Hikida RS, Staron RS, Hagerman FC, Walsh S, Kaiser E, Shell S, Hervey S. Effects of high-intensity resistance training on untrained older men. II. Muscle fiber characteristics and nucleo-cytoplasmic relationships. J Gerontol A Biol Sci Med Sci. 2000;55(7):B347–354. [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell RT, Whitelaw N, Bazzarre T. Best-practice physical activity programs for older adults: findings from the national impact study. Am J Public Health. 2009;99(2):362–368. doi: 10.2105/AJPH.2007.131466. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Kalapotharakos VI, Diamantopoulos K, Tokmakidis SP. Effects of resistance training and detraining on muscle strength and functional performance of older adults aged 80 to 88 years. Aging Clin Exp Res. 2010;22(2):134–140. [PubMed] [Google Scholar]
- Kamen G, Knight CA. Training-related adaptations in motor unit discharge rate in young and older adults. J Gerontol A Biol Sci Med Sci. 2004;59(12):1334–1338. [PubMed] [Google Scholar]
- Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;(3):CD002759. doi: 10.1002/14651858.CD002759.pub2. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Manini TM, Clark BC. Dynapenia and Aging: An Update. J Gerontol A Biol Sci Med Sci. 2011 doi: 10.1093/gerona/glr010. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Manini T, Marko M, VanArnam T, Cook S, Fernhall B, Burke J, Ploutz-Snyder L. Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life. J Gerontol A Biol Sci Med Sci. 2007;62(6):616–623. [PubMed] [Google Scholar]
- Manini TM, Russ DW, Clark BC. The complex relationship between muscle mass and muscle strength. In: Cruz-Jentoft AJ, Morley JE, editors. Sarcopenia. Chichester, U.K.: John Wiley & Sons, Ltd; 2012. pp. 74–103. [Google Scholar]
- Narici MV, Maffulli N. Sarcopenia: characteristics, mechanisms and functional significance. Br Med Bull. 2010;95:139–159. doi: 10.1093/bmb/ldq008. [PubMed] [CrossRef] [Google Scholar]
- NCOA. Best Practices in Physical Activity. Washington, D.C.: The National Council on Aging; 2004. Retrieved from http://www.ncoa.org/improve-health/center-for-healthy-aging/content-library/BP_PhysicalActivity.pdf. [Google Scholar]
- NIA. Go4Life. 2015 Retrieved April 6, 2015, from https://go4life.nia.nih.gov.
- Peterson MD, Rhea MR, Sen A, Gordon PM. Resistance exercise for muscular strength in older adults: a meta-analysis. Ageing Res Rev. 2010;9(3):226–237. doi: 10.1016/j.arr.2010.03.004. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Peterson MD, Sen A, Gordon PM. Influence of resistance exercise on lean body mass in aging adults: a meta-analysis. Med Sci Sports Exerc. 2011;43(2):249–258. doi: 10.1249/MSS.0b013e3181eb6265. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Physicians, American Academy of Family. Choosing Wisely: Don’t prescribe under-dosed strength training programs for older adults. Instead, match the frequency, intensity, and duration of exercise to the individual’s abilities and goals. 2015 Retrieved March 23, 2015, from http://www.aafp.org/afp/recommendations/viewRecommendation.htm?recommendationId=210.
- Program on Healthy Aging, School of Rural Public Health, Texas A&M Health Science Center. Exercise And Screening for You. 2008 Retrieved April 28, 2015, from http://www.easyforyou.info/aboutus.asp.
- Reeves ND, Maganaris CN, Narici MV. Effect of strength training on human patella tendon mechanical properties of older individuals. J Physiol. 2003;548(Pt 3):971–981. doi: 10.1113/jphysiol.2002.035576. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Rosenberg IH. Summary comments. Am J Clin Nutr. 1989;50:1231–1233. [Google Scholar]
- Russ DW, Gregg-Cornell K, Conaway MJ, Clark BC. Evolving concepts on the age-related changes in “muscle quality” Journal of cachexia, sarcopenia and muscle. 2012 doi: 10.1007/s13539-011-0054-2. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Sayer AA, Robinson SM, Patel HP, Shavlakadze T, Cooper C, Grounds MD. New horizons in the pathogenesis, diagnosis and management of sarcopenia. Age Ageing. 2013;42(2):145–150. doi: 10.1093/ageing/afs191. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Singh NA, Quine S, Clemson LM, Williams EJ, Williamson DA, Stavrinos TM, Singh MA. Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: a randomized controlled trial. J Am Med Dir Assoc. 2012;13(1):24–30. doi: 10.1016/j.jamda.2011.08.005. [PubMed] [CrossRef] [Google Scholar]
- Starkey DB, Pollock ML, Ishida Y, Welsch MA, Brechue WF, Graves JE, Feigenbaum MS. Effect of resistance training volume on strength and muscle thickness. Med Sci Sports Exerc. 1996;28(10):1311–1320. [PubMed] [Google Scholar]
- Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Vassileva MT. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69(5):547–558. doi: 10.1093/gerona/glu010. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Sylliaas H, Brovold T, Wyller TB, Bergland A. Progressive strength training in older patients after hip fracture: a randomised controlled trial. Age Ageing. 2011;40(2):221–227. doi: 10.1093/ageing/afq167. [PubMed] [CrossRef] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [PubMed] [CrossRef] [Google Scholar]
- Van Roie E, Delecluse C, Coudyzer W, Boonen S, Bautmans I. Strength training at high versus low external resistance in older adults: effects on muscle volume, muscle strength, and force-velocity characteristics. Exp Gerontol. 2013;48(11):1351–1361. doi: 10.1016/j.exger.2013.08.010. [PubMed] [CrossRef] [Google Scholar]
- Visser M, Schaap LA. Consequences of sarcopenia. Clin Geriatr Med. 2011;27(3):387–399. doi: 10.1016/j.cger.2011.03.006. [PubMed] [CrossRef] [Google Scholar]
- Willardson JM. A brief review: factors affecting the length of the rest interval between resistance exercise sets. J Strength Cond Res. 2006;20(4):978–984. doi: 10.1519/R-17995.1. [PubMed] [CrossRef] [Google Scholar]
- Willoughby DS. Current Comments are official statements by the American College of Sports Medicine concerning topics of interest to the public at large. Indianapolis, IN: American College of Sports Medicine; 2015. Resistance Training and the Older Adult ACSM Current Comment. [Google Scholar]
